Ensuring accurate and timely verification of patient eligibility and benefits is critical in today’s healthcare landscape. At finnastra, we provide comprehensive eligibility & benefits verification services to simplify the verification process, reduce errors, and support seamless medical billing. By utilizing cutting-edge technology and a dedicated team of experts, our solutions enhance efficiency and accuracy, enabling healthcare providers to focus on delivering quality patient care.
Choosing the right partner for eligibility & benefits verification services can significantly impact your practice’s operational success. With years of experience, we understand the nuances of insurance verification and benefits assessment. Our team ensures that every detail is meticulously checked, reducing claim denials and payment delays. Our commitment to transparency, accuracy, and customized solutions sets us apart as a trusted partner in the healthcare sector.
Our eligibility & benefits verification services are designed to address the unique needs of healthcare providers, offering:
1. Real-Time Verification: We provide immediate updates on patient eligibility and benefits to streamline appointment scheduling and billing.
2. Comprehensive Data Collection: From insurance coverage to co-payments, our services include a thorough assessment of all critical data.
3. Advanced Technology Integration: Leveraging state-of-the-art tools ensures accuracy and reduces manual errors.

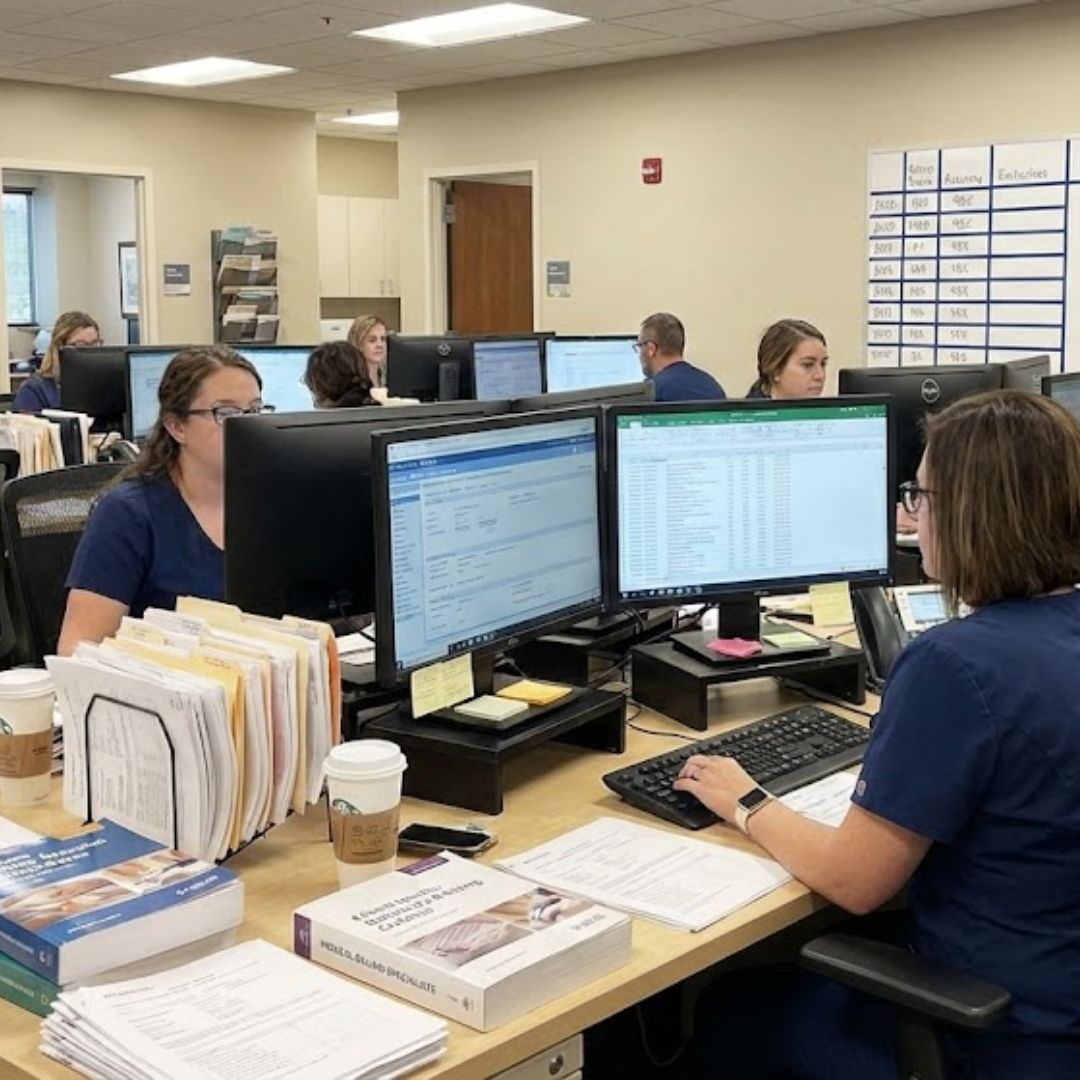
4. Expert Team Support: Our skilled professionals are trained to handle complex verification processes efficiently.
5. HIPAA Compliance: We prioritize patient data security, adhering to strict confidentiality standards.
6.Customized Solutions: Tailored services to meet the specific needs of clinics, hospitals, and other healthcare providers.
Accurate eligibility & benefits verification offers a multitude of advantages for healthcare providers:

Verifying patient details before appointments minimizes rejections due to errors or omissions.

Timely and accurate verification ensures faster reimbursements, improving financial stability.

Clear communication regarding coverage and out-of-pocket expenses fosters trust and satisfaction.

Automation and expert support reduce administrative burdens, allowing staff to focus on core tasks.

Ensuring data integrity and adherence to legal standards protects against liabilities.

Our streamlined process for eligibility & benefits verification services involves the following key steps:

Gathering all necessary patient and insurance information, including demographic details and policy numbers.
Contacting insurance providers to confirm coverage details, eligibility, and benefits.
Assessing deductibles, co-pays, co-insurance, and exclusions for comprehensive insights.

Providing healthcare providers with immediate access to verified information.

Addressing any discrepancies and re-verifying details as required to ensure accuracy.

Delivering detailed reports that support decision-making and streamline billing processes.
Partnering with us for eligibility & benefits verification services guarantees a reliable and efficient approach to managing patient information. Our services are tailored to fit diverse healthcare needs, from small clinics to large hospital systems. By choosing us, you gain a partner committed to enhancing your operational success while maintaining the highest standards of quality and security.
Whether you’re seeking to reduce administrative costs, improve claim approvals, or elevate patient satisfaction, we’re here to help. Together, we can ensure that your practice runs smoothly and your patients receive the care they deserve without unnecessary delays.
Eligibility and benefits verification is a cornerstone of efficient healthcare management. With our robust eligibility & benefits verification services, you can rely on precise, timely, and secure solutions tailored to your practice’s needs. Experience the difference of working with a trusted partner who prioritizes your success and patient satisfaction. Reach out today to learn more about how we can support your eligibility and benefits verification needs.