Credentialing plays a crucial role in ensuring healthcare professionals meet the required standards to deliver quality medical services. At Finnastra, we provide structured and reliable physician credentialing services that verify qualifications, training, and professional history to streamline the enrollment process. Our approach helps healthcare providers gain timely access to payer networks while maintaining full compliance with regulatory requirements.
Our scope also extends to provider credentialing services for medical groups, clinics, and hospitals. We work directly with administrative teams to manage the complexities of documentation and strict submission timelines. This reduces the risk of delays and ensures providers can start offering patient care without unnecessary interruptions.
Selecting the right partner for physician credentialing services ensures accuracy, transparency, and faster turnaround times. Our team applies healthcare-specific knowledge and a methodical process to address every credentialing requirement with precision. From solo practitioners to multi-specialty groups, we provide scalable solutions to meet diverse needs.
With our provider credentialing services, compliance is never left to chance. We align every step of the process with payer expectations, regulatory standards, and internal timelines. This attention to detail allows us to remain a trusted partner for organizations seeking consistent results.

Our medical credentialing services are designed with careful attention to detail, covering all essential verification steps. This includes primary source checks for education and training, license validations, DEA certification confirmations, malpractice coverage verification, and hospital privilege reviews. Every stage is tailored to meet payer and accreditation body requirements.
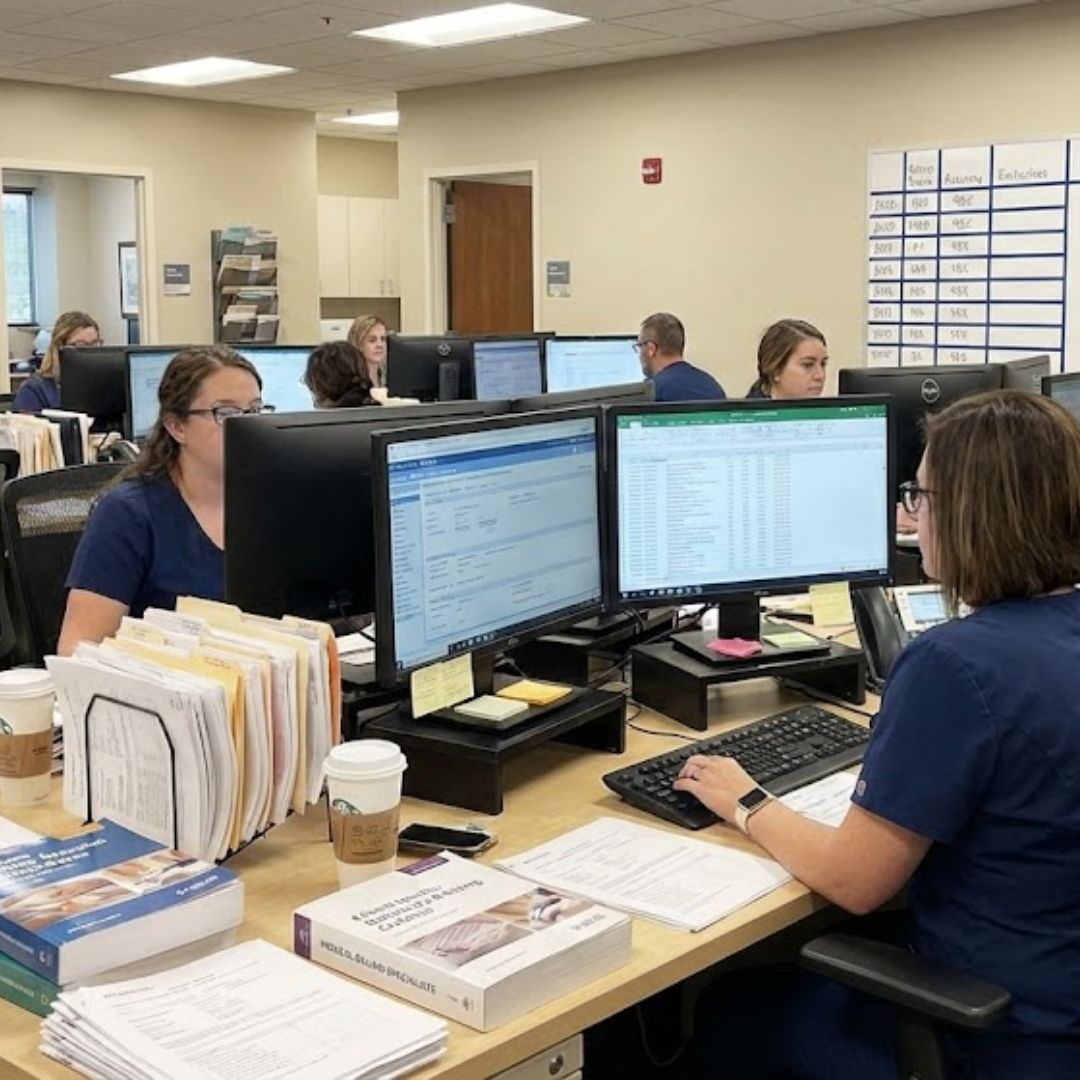
We optimize provider credentialing services by centralizing the workflow. Our team handles form preparation, payer communications, status tracking, and frequent updates. By leveraging secure portals, automation tools, and dedicated account managers, we deliver a streamlined process from start to finish.
Lifetime credentialing support, Once your setup is complete, credentialing is fully covered for the lifetime of our partnership, no hidden fees, ever.
Getting credentialed with payers is often a long and complex process. We take care of initial credentialing for new providers as well as re-credentialing to maintain your active status with insurance networks. Our experts ensure that all applications are accurately prepared, submitted on time, and followed up with until approvals are finalized, helping you avoid costly delays in reimbursement.
CAQH ProView is a crucial tool for credentialing, but keeping it updated can be tedious. Our team manages the entire CAQH setup process, ensuring that your profile is correctly built, attested, and kept current. We also handle routine updates and re-attestations, reducing the risk of payer denials caused by outdated or incomplete information.
Knowing where you stand with payer panels is essential. We provide real-time tracking of your panel status, so you’re always informed about approvals, pending applications, and renewals. Our specialists maintain direct communication with insurance companies and payers to address issues, clarify requirements, and expedite approvals, taking the burden off your shoulders.
Credentialing is not just about getting on panels; it’s also about securing the best possible reimbursement rates for your services. Our team reviews and negotiates payer contracts on your behalf, ensuring you receive fair and competitive compensation. With expert negotiation, we help maximize your revenue potential and strengthen your long-term payer relationships.
Missing a license renewal or government portal update can disrupt your practice. We provide proactive license expiration tracking to ensure your credentials are always valid and up to date. Additionally, we manage your records in key government systems such as NPPES, PECOS, and other required portals, ensuring compliance and smooth operation without administrative hassles.

A well-executed credentialing process offers more than just compliance—it protects revenue streams and builds credibility. Efficient healthcare credentialing services support faster payer approvals, reduce the likelihood of denials, and establish trust with patients and industry partners.
Our structured methods for provider credentialing services help organizations maintain their professional image while ensuring all providers meet required qualifications. This results in uninterrupted service delivery, smoother reimbursement cycles, and stronger relationships with both patients and payers.
We follow a systematic process to ensure accuracy and compliance at every stage. The first step in our physician credentialing services involves gathering detailed information from the provider, including credentials, licenses, and professional history. This is followed by thorough verification with official sources to confirm accuracy.
For provider enrollment services, we compile verified data into payer-specific formats and submit them to insurance carriers, Medicare, Medicaid, and hospital networks. Our team also manages ongoing communications with payers, addressing missing documentation or clarifications until full approval is secured.
Once credentialing is complete, we maintain proactive monitoring to prevent lapses. Alerts for license renewals and re-credentialing deadlines are part of our ongoing support, ensuring providers remain active with all networks and regulatory boards.
Managing insurance requirements can be complex for healthcare providers, especially when working across multiple payers. Our insurance credentialing services are designed to simplify this process by managing direct communications with carriers, verifying plan-specific requirements, and resolving discrepancies quickly. We ensure every submission meets payer-specific standards to avoid costly delays.
Alongside this, our provider enrollment services facilitate new practice launches, staff expansions, and network participation changes. Whether adding a new provider or updating existing records, we handle each stage efficiently to maintain compliance.

Partnering with us for medical credentialing services means working with a team that prioritizes compliance, efficiency, and accuracy. We take on the administrative burden so healthcare professionals can focus on delivering care rather than navigating paperwork and follow-ups.
Through our healthcare credentialing services, we offer a combination of advanced technology, industry expertise, and personal support. Each solution is adaptable to the size and scope of the healthcare organization, from independent practices to large hospital systems.
Credentialing is not a one-time process; it requires ongoing management. Our provider credentialing services include monitoring for renewals, maintaining updated records, and ensuring timely re-submissions when regulations or payer requirements change. This proactive approach reduces the risk of interruptions in patient care or reimbursement.
We also provide extended support through insurance credentialing services, making sure that provider data stays accurate and up to date across all payer systems. This consistency protects both revenue cycles and professional reputations.
Over time, maintaining a well-credentialed team becomes a key factor in operational stability. Our provider enrollment services and verification systems are built to grow with your organization, adapting to new provider additions, expanded service lines, or evolving payer requirements. By keeping credentialing processes centralized and transparent, we help ensure long-term compliance and efficiency.
Working with Finnastra means gaining a partner committed to accurate documentation, timely approvals, and dependable communication at every step of the credentialing journey.